|
| HOME | THIS ISSUE | CALENDAR | GRANTS | BACK ISSUES | < BACK | NEXT > |
Grad student first to complete master’s in clinical, translational research by Cindy Weiss - February 19, 2008 |
||||
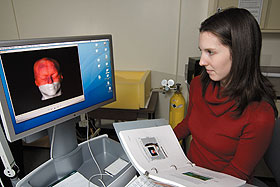
| The first master’s degree student in a new Storrs campus-Health Center program has successfully defended her thesis, a milestone for a collaborative effort that aligns the University with the National Institutes of Health “Roadmap” for the direction of medical research. Colleen Jackson completed her master’s degree in clinical and translational research in late January. A psychology student continuing toward her Ph.D. in clinical neuropsychology, she took her coursework and defended her thesis at the UConn Health Center, where she was one of five students in various stages of the new master’s program. Three others are physicians – two are junior faculty members in pediatrics from the Children’s Medical Center and Department of Psychiatry at the Health Center, and the other a Health Center fellow in urogynecology. The fifth is another psychology graduate student. The clinical translational master’s degree is designed to bridge a gap between research and practice, reflecting an NIH priority to speed, streamline, and improve the delivery of research findings to patient care and encourage innovation. Physicians typically do not receive formal training in research, says Dr. Anne Kenny, associate professor of medicine at the Health Center and co-director of the master’s degree program. And researchers need to learn to carry new discoveries through clinical trials and out to patients, says the other co-director, Peter Snyder, professor of clinical neuropsychology and cognitive neuroscience in the College of Liberal Arts and Sciences and the medical school’s Department of Neurology. The new master’s degree addresses both needs and is expected to attract physicians, medical and dental students, and graduate or post-doctoral students in psychology, nursing, pharmacy, bioengineering, and other fields. The degree is not terminal but can be completed as part of an MD, DDS, or Ph.D. program, or as post-doctoral training. Physicians can work on the degree part-time over two or three years. The program is taking applications from doctors affiliated with UConn at Hartford and St. Francis hospitals as well as the Health Center. Offering a clinical and translational degree strengthens UConn’s hand in applying for an NIH Clinical and Translational Science Award (CTSA), a major award for universities with medical centers. The NIH estimates that total funding for CTSA awards around the country will be $574 million over about five years. So far, 24 academic health centers in 18 states have received them. Training in an area that is such a national priority means that “graduates are going to be a very desirable commodity,” says Professor Charles Lowe, head of the psychology department. Career tracks available for people trained in clinical and translational research include academia, research careers with pharmaceutical companies and government agencies, and working for social programs or non-governmental organizations. “You need the knowledge base to go from textbook to application,” says Snyder. Jackson, a native of a Chicago suburb, did undergraduate research at the Beckman Institute for Advanced Science and Technology at the University of Illinois at Urbana-Champaign. She wanted to continue in research as a graduate student but also keep a clinical focus.
Her master’s degree work involved preparing a thorough literature review on what is known about biomarkers for Alzheimer’s disease. Biomarkers would enable clinicians to identify people at risk for Alzheimer’s before they show symptoms. Her review paper was accepted without revision by the Journal of Alzheimer’s Disease and was published in January. She also prepared a proposal for a pre-doctoral grant from NIH. Her Ph.D. work will carry forward her research proposal on Alzheimer’s. Bringing the fruits of research on Alzheimer’s into clinical practice is particularly important, says Snyder, as baby boomers grow into old age. More than 24 million people around the world are now estimated to have Alzheimer’s disease, and that number is expected to grow to 81 million by the year 2040. Researchers who develop grant-getting skills and learn how to interact with clinicians in industry will have a competitive advantage, and those are areas that the new master’s degree covers, says Snyder. Students in the new degree program typically take three core courses and a series of electives. They learn the history of clinical research, ethics, modern research methodology, and advanced biostatistics, among other things. They also learn practical skills – grant writing, partnering with industry sponsors, corresponding with journal editors, and creating slide presentations. Training in biostatistics and modern statistical modeling is particularly important because of the massive amounts of available data – much of it confidential – that must be managed in clinical research, says Snyder. As many as 54 faculty members at the Health Center and the Storrs campus have agreed to teach or mentor students in the program. The program formalizes what some physicians previously learned “by hook or by crook,” searching out mentors to guide them in research. Many students do not want to pursue a double degree – Ph.D. and MD – because it takes so long, says Kenny: “This way they can blend research, clinical care, and teaching.” Research opens a creative pathway and new options, she says. “It’s a whole different way to attack a problem, without a patient before you.” As many as 50 percent of the physicians who start out teaching at academic medical centers are not there five years later, she says, because they don’t see opportunities to combine research with teaching and clinical work. This program would give them a foothold for learning how to do research and get into it. |
| ADVANCE HOME |